The application of hyperbaric oxygen therapy (HBOT) to chronic traumatic brain injury (TBI) can be traced to clinical practice and research in South Florida and New Orleans, Louisiana. It is well known that the practice of HBOT in chronic neurological conditions was pioneered by the late Dr. Richard Neubauer in the 1970s. Beginning with a serendipitous finding of gratuitous neurological improvement in two multiple sclerosis patients undergoing HBOT for chronic bone infections, Dr. Neubauer began applying HBOT to patients with other neurological conditions, primarily stroke. In 1994, he published his first case of HBOT treatment of chronic TBI in the Southern Medical Journal.
New Orleans – The Sentinel Cases
In New Orleans, the first application of HBOT to chronic TBI began with a project initiated by Drs. Keith Van Meter and Sheldon Gottlieb in boxers with dementia pugulistica. Drs. Van Meter and Gottlieb obtained a small grant from the Hirsch Foundation in 1989 to study HBOT and SPECT brain imaging in brain injured Louisiana boxers. Due to a series of events and coincidences, the project was absorbed into my practice which was investigating and treating acute spinal cord injuries and sub-acute brain decompression illness in one of our New Orleans area hyperbaric departments. While the grant only allowed for the treatment of two boxers, we were able to see limited improvement in both boxers, one whose injury was approximately 1 year old and the other whose injury was over 23 years after his last bout. The first boxer experienced improvement in his dizziness and the second, a paranoid schizophrenic demented patient, became more alert, socially engaging, less depressed, and registered some mild improvements on cognitive testing.
At the same time the boxers were receiving treatment, I began applying a low pressure protocol similar to the ones used by Dr. Halbach and Dr. Neubauer in acute and chronic neurological conditions, respectively, to our divers with subacute and chronic brain decompression illness and a case of acute TBI in 1990. The acute TBI case can be viewed on YouTube and above. This is the Chad Rovira case which can also be seen in K.K. Jain’s The Textbook Of Hyperbaric Medicine, 3rd, 4th, and 5th Editions, and in my book, The Oxygen Revolution. Chad was a 18 year old college freshman who was sniffing an organic solvent called ethyl chloride, aka “Head Cleaner”, with friends as they were driving on Interstate 10 at 2:30 in the morning. Due to a dare and sudden jerk of the car as Chad was climbing out one of the windows when he was catapulted onto the pavement at 70 mph. Gathered up by his friends he was brought three miles down the highway to our emergency department, apneic, with a Glasgow Coma Scale of 6. When I arrived for my ED shift at 7a.m., he was on the ventilator and unresponsive to deep pain. As I walked past him, I stopped and remarked to the nurses that in five years I would be able to treat him acutely and emergently with HBOT. That musing turned out to be wildly optimistic, but seemed reasonable at the time.
Little did I know that Chad’s father was a veterinarian and friends with multiple staff physicians at our hospital. Within hours I was approached by a group of surgeons, internists, and the family to see if HBOT could ameliorate Chad’s brain injury. The week prior to this accident I had given a lecture to the medical staff on the application of a lower pressure protocol of HBOT to divers with cerebral DCI. Impressed by the SPECT brain imaging and case reports, the physicians recommended HBOT to the Rovira family. After presenting the literature to Dr. Rovira and discussing HBOT effects on subarachnoid hemorrhage, basilar skull fracture, contusions, and subdural hematoma (Chad’s four diagnoses), I began treating Chad at 10 p.m. that night, over 19 hours after his accident.
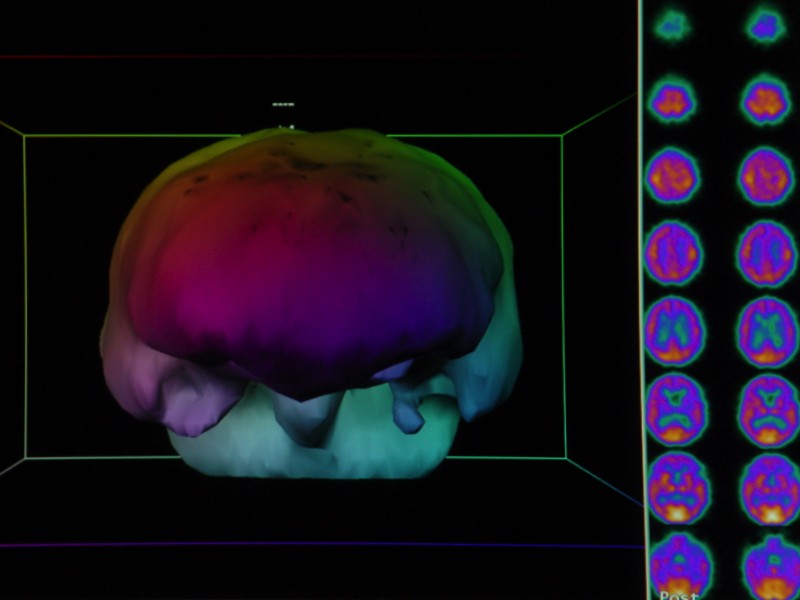
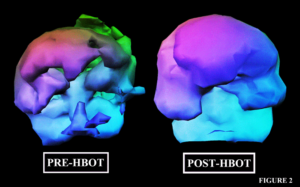
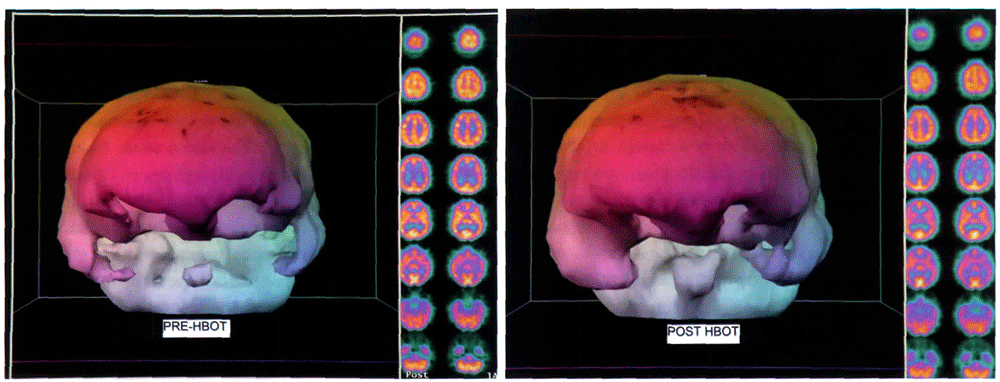
As can be seen on the video during the first HBOT, Chad began to show signs of increased neurological activity when he bucked the ventilator at depth, necessitating IV Ativan. With each successive treatment his neurological condition improved. Wanting to capture his progress on functional imaging, I obtained a SPECT brain scan on the single-headed camera we had at the hospital. It was read by an experienced radiologist as normal, yet Chad was still on a ventilator.As is so often the case when the functional imaging doesn’t match the condition of the patient, there was a technical explanation. In this case, it was the low resolution of the scanner (See Figure 1). Within one week of that scan, I transferred Chad by ambulance to West Jefferson Medical Center in Marrero, Louisiana, where we had the high resolution triple-head scanner. The first scan (see Figure 2 below) showed in dramatic fashion the injury which was so apparent clinically. Approximately 9 days later the scan was repeated after a single HBOT, showing the major effect one HBOT had on brain blood flow and metabolism. (The imaging on the cover is a three dimensional reconstruction of the outer surface of the brain blood flow scan. The reader is looking at the patient face on. Irregularity of the surface is abnormal, as are “holes” which are significant reductions in blood flow).
As treatment progressed, Chad was extubated and transferred to a nearby subacute neurological treatment center from which he was able to continue outpatient HBOT at our facility. By the 10th week, he was walking and talking, an achievement marveled at by his neurosurgeons and all of his caregivers. His repeat brain scan is the second scan in Figure 2. Chad was then transferred to a highly respected neurorehabilitation facility in New Orleans and all HBOT ceased because of the negative statements made by his new caregivers. Three months after his transfer, his father phoned me to report that Chad had made some modest gains in the first two weeks after transfer, but then ceased to improve any further. My initial reaction was that the obvious culprit was the discontinuance of HBOT. The time-honored practice of medicine is to continue a therapy until a patient no longer shows a positive response to that therapy. In Chad’s case, neurological improvement was a sharply up-sloped curve that was interrupted by transfer to a facility that would not allow continuation of the therapy that had been responsible for his current condition. An alternate explanation was that the subarachnoid hemorrhage might be responsible for developing hydrocephalus, as it does in a small percentage of patients. I performed an evaluation at the request of Dr. Rovira and then referred him for an independent neurosurgical opinion which revealed no hydrocephalus. Dr. Rovira then requested re-institution of the HBOT at the outpatient clinic near New Orleans.
 Before restarting HBOT, it was critically important to structure Chad’s case so that there could be no denying the previous positive impact of HBOT and the likely additional positive impact of the next round of HBOT. Single case studies can draw causal conclusions, especially when the design follows the A-B-A design where therapy A is delivered to the subject, then withdrawn while control period B proceeds, after which therapy A is re-introduced. If the patient and therapist are blinded or the patient is unable to appreciate the intent of the therapy/lacks insight into the purpose of the therapy, the design is stronger. In Chad’s case, neither the therapist nor the patient were blinded, but the patient lacked insight. In addition, every one of the caregivers at the rehabilitation hospital had been so infused with negative information about HBOT and its contribution to Chad’s current condition that Chad’s evaluations were performed with an extremely negative bias, essentially a negative placebo effect.
Before restarting HBOT, it was critically important to structure Chad’s case so that there could be no denying the previous positive impact of HBOT and the likely additional positive impact of the next round of HBOT. Single case studies can draw causal conclusions, especially when the design follows the A-B-A design where therapy A is delivered to the subject, then withdrawn while control period B proceeds, after which therapy A is re-introduced. If the patient and therapist are blinded or the patient is unable to appreciate the intent of the therapy/lacks insight into the purpose of the therapy, the design is stronger. In Chad’s case, neither the therapist nor the patient were blinded, but the patient lacked insight. In addition, every one of the caregivers at the rehabilitation hospital had been so infused with negative information about HBOT and its contribution to Chad’s current condition that Chad’s evaluations were performed with an extremely negative bias, essentially a negative placebo effect.
A complete set of evaluations were performed: physical, occupational, emotional, and cognitive. The main impediment to further gains in neurorehabilitation was identified by the care team as the patient’s lack of insight into his injury. Despite spastic gait and right arm, poor balance, impaired speech and cognition, and inpatient status at a rehabilitation hospital, Chad was convinced that he was normal, had suffered no residual effects of his injury, and was going back to college where he would achieve his goal of becoming an orthopedic surgeon. SPECT brain imaging was repeated before and after a single HBOT to test responsiveness of his brain to additional therapy. The images revealed an interim progression to infarct in the right hemisphere in the previous five months since his last HBOT, some deterioration in other areas of the brain, but an improvement after the single HBOT. Again, the images are presented in the 5th Edition of the Textbook of Hyperbaric Medicine, Chapter 19.
Treatment commenced, essentially an A-B-A study design, and Chad began to improve until an emergent phone call to me from the rehabilitation center claiming a sudden deterioration in Chad’s condition. Caregivers had noted profuse sweating and a significant rise in blood pressure while Chad was playing tennis. Inadvertently, they also mentioned that he was no longer restricted to his tricycle, having progressed to riding a bicycle. Despite this progression of physical ability they reported that Chad was very depressed over his realization that he was not capable of becoming an orthopedic surgeon. They attributed all of these “negatives” to the HBOT and requested an immediate cessation of further HBOT.
What’s wrong with this picture? A skilled tennis player prior to head injury, unable to play tennis post injury due to poor balance and coordination, is now playing tennis again? Improved balance such that he had graduated from a tricycle to a bicycle, and “depression” over his new insight into his injury and the realization that he was likely not going to be able to fulfill his dream of becoming an orthopedic surgeon? Lastly, sweating during a tennis match in the late May heat and humidity of New Orleans and recorded hypertension in the middle of such exercise? I called for a “care conference” where I sat down and faced the hostile contingent of therapists to try to make sense of the above nonsense. With Dr. Rovira in attendance, the conclusion was that Chad had made significant gains and finally surmounted the greatest barrier to further improvement, lack of insight. Treatment continued.
The goal of HBOT was clinical plateau. Chad declared this when he kept insisting that “Dr. Harch, the math is back in my head. I am able to do math again and I want to go back to college.” At that point I stopped his treatment. We were in the neighborhood of 80 additional treatments (a future key figure). At his exit video, I asked Chad a key question to test his insight, “So, Chad, do you believe that you have no brain damage?” No sooner had I uttered the words and his hand came up immediately to correct me, “Dr. Harch, excuse me, I don’t have brain damage, I have a brain injury.” How inappropriate my word choice, but to be corrected so quickly and INSIGHTFULLY by a patient who had had such a devastating injury. I stood corrected and in amazement of his transformation. With this one sentence, I realized that there was no need for all of the retesting that was to follow. That testing showed physical, emotional, occupational, and cognitive gains, with the most impressive change being a 40 percentile improvement in written computational math. This was far greater than a standard deviation improvement in just a few short months.
Chad was subsequently discharged from the neurorehabilitation hospital, returned to college part-time, and was hired by a bank under a special program. His performance at the bank was so impressive that he was re-hired as a normal employee, promoted, and has been an integral part of the credit analysis department for the last 14 years.
While Chad’s case is remarkable and clearly fits the A-B-A single case causality/proofing design, it was just one of a series of phenomenal patients (cases) I had the privilege of treating in the late 1980s and early 1990s. It was these cases, the boxers, divers, acute spinal cord injury, and traumatic brain injury cases who all presented at the same time and who were responsible for the development of the 80 HBOT 1.5 protocol that followed. Had I chosen to abide by the rules of reimbursement and rigidity of the narrow list of hyperbaric indications, I never would have experienced the success of these cases. Instead, I followed simple principles of medical practice, in particular, the principles embodied in the Hippocratic method which states that “I will prescribe regimen for my patients …” That regimen, however non-traditional, was dictated by previous science and some reports of other physicians’ experiences, particularly Dr. Neubauer’s. It was this freedom of choice in medicine in a remote area of Southeast Louisiana through the collective experience of a combination of patients that changed my life and career.
From Clinical Experience to Scientific Meetings
By 1991, the collection of cases generated word-of-mouth referral of other chronic stroke, TBI, cerebral palsy, pediatric and adult neurological patients. In 1994, at the UHMS Annual Meeting in Denver, Colorado, I reported three retrospective case series abstracts: 13 divers with subacute and chronic cerebral DCI, 23 acute, subacute, and chronic carbon monoxide poisoned patients, and 18 patients with chronic ischemic, hypoxic, or traumatic brain injury. All of the patients had pre/post high resolution SPECT brain imaging and cerebral conditions with primarily damage to the white matter. Twelve of the eighteen patients in the 1/H/TBI abstract were chronic TBI patients and nearly all of them were moderate to severe TBI.
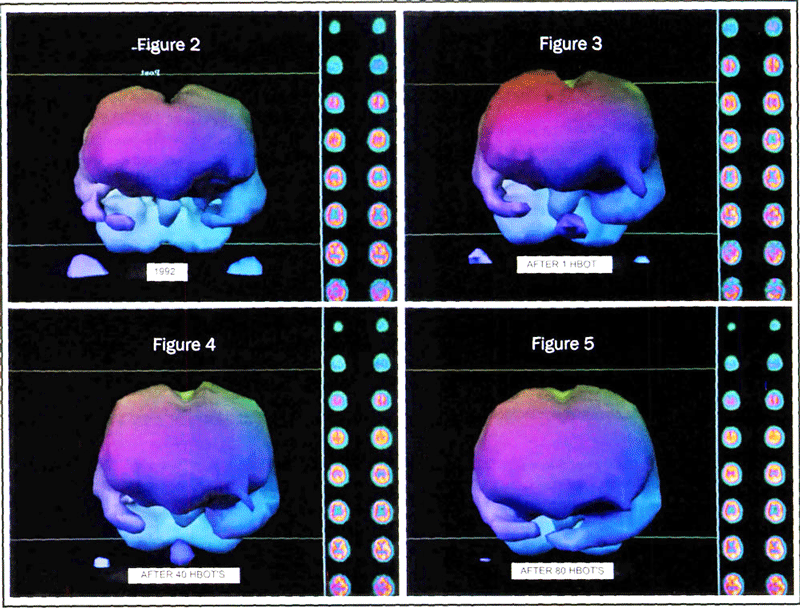
The first of these chronic TBI patients was one of the most instructive, a 25 year old woman referred by her high school friend, one of the boxers whom we evaluated but did not treat. She was 5.5 years out from a motor vehicle accident that delivered a severe TBI. Taken to multiple rehabilitation hospitals, she was still severely impaired. The scan-dive-scan sequence revealed an abnormal brain that responded to a single HBOT. Over the course of the next five months of HBOT she made physical, emotional, behavioral, and cognitive gains that were consistent with her functional brain imaging and the entries from her journal at the beginning and middle points of her therapy. Her case was presented in the 2nd-5th editions of the Textbook of Hyperbaric Medicine and are reproduced here. [Figure 2 is the three dimensional surface reconstruction of her pre-HBOT SPECT scan. Figure 3 was after the first HBOT (The Neubauer SPECT Sequence), Figure 4 after 40 Treatments (half the Harch Protocol), and Figure 5 after the 80 Treatments, (the Harch Protocol)].
The other 11 chronic TBI patients had similar stories and responses. Some of their cases are in other publications. All of them were documented by high resolution functional brain blood flow imaging and some by cognitive testing. Most importantly, the patients were much improved clinically and their lives changed for the better. What had also become apparent was that improvements were measurable and unequivocally obvious to independent observers, i.e., caregivers, by the time patients reached 80 low pressure treatments. We had started with 40 treatments upon a seemingly casual response by Dr. Neubauer to my question regarding the number of treatments necessary to see a durable measurable improvement in patients. At the conclusion of 40 treatments I could discern clinical improvements and the imaging would document this, however, it was not as evident to the patients or their families because the 40 treatments were spread over seven weeks. Most observers could see improvements in the patients, especially when I showed them before and after videos of the patients’ neurological exams, but it was not as prominent as after 80 treatments.
Replicating the Human Experience in an Animal Model
Surprisingly, the reaction to these retrospective case series at the 1994 meeting was rather negative. One of the criticisms was that the cases were not believable because they were chronic; that they would be credible if I could duplicate the effect in an animal model. For a clinician, this is ludicrous. A clinical response in a patient with a chronic, unchanging medical condition that has resisted all previous therapies is much more believable than any mechanistic study in animals. Nevertheless, I sought an animal model to attempt to duplicate the human experience. Specifically, the improvements in brain blood flow seemed congruous with the HBOT angiogenesis model of Robert Marx in head and neck radiation necrosis, the improvements in transcutaneous oxygen measurements in chronic peripheral vascular ulcers and diabetic foot ulcers, and even the angiogenesis effects of HBOT in acute burns and compromised flaps and grafts.
A preemptive review of the medical literature for this animal study was both shocking and informative. My searching failed to produce an animal model of chronic TBI or any literature on therapies in chronic TBI. In the history of traumatic brain injury research, no one had devoted time or resources to treating chronic TBI. It is as if the condition did not exist. As a solution, I decided to take a well characterized acute traumatic brain injury model and allow the animals to live with a maturing injury. The perfect model was provided by the open focal cortical contusion model of Feeney, first developed in 1979. In this model, a small piece of parietal skull bone is removed and a 20g weight is dropped through a metal guide tube 20 em onto the dura/brain of a rat. The animal is allowed to recover. By 30 days, infarction is complete in the cortex, while the underlying microscopic contusion in the hippocampus continues. The cortical infarct causes a defect in opposite forelimb placing. The hippocampal contusion causes a defect in spatial learning and memory that continues to decline over the next 270 days. The spatial learning and memory defect is captured by a well-known cognitive test called the Morris Water Task in which rats are tested to find and remember the location of a plexiglass platform buried just beneath the surface of a tub filled with opaque liquid. Using visual cues on the wall of the tub room, rats learn to locate the buried platform. The plan was to apply the human protocol to the rats during the 270 day decline in learning, see if the rats could reverse their cognitive injury, and section their brains to see if angiogenesis was associated with any improvement in memory.
In the first run of the experiment, 12 rats were divided into three groups of four which received either 40 treatments, 80 treatments, or 40 sham air treatments. When the two HBOT groups were combined, the results showed significant improvements in spatial learning/memory and blood vessel density after HBOT. The results were presented at the 1996 UHMS meeting. Subsequent iterations of the experiment used a sham air control group, an 80 HBOT group, and an altitude control group that stayed in the lab in Albuquerque while the other groups made the round trip to New Orleans. The results were statistically stronger and again showed an improvement in spatial learning and memory with a significant increase in vascular density in the hippocampus. The vascular density and improved memory were highly correlated. The study was published in 2007 in Brain Research. 1174:120-129.
Implications of the Animal Study on HBOT 1.5
The implications of this study were profound. To our investigation, this was the first improvement in chronic brain injury in the history of science, but more importantly, it replicated the human experience we had seen in the boxers and other chronic brain injured patients. Normally, the FDA approval process for drugs starts with in vitro experiments and proceeds to small animals, large animals, primates, foreign human studies, and finally clinical trials in the U.S. We had been treating patients for years, documenting clinical and functional brain imaging improvements, yet had to revert to an animal model to demonstrate proof at a hyperbaric medical society meeting. The greater good that came out of this, however, was the confirmation of the lateralization of this TBI proofing/effectiveness to other causes of chronic brain injury that we had been investigating in the previous years.
Extension of TBI Proofing to other Neuropathologies: The Perfusion/Encephalopathies Study
This lateralization process began with the simple notion that chronic wounding in the body was stereotypic regardless of location and possible etiology. In other words, a chronic wound in the foot should have similar pathology to a chronic brain wound, and a chronic brain wound due to TBI should have similar pathology to a chronic brain decompression illness wound. While the argument is not perfect with respect to the type of primary insult, the underlying principle was that there were more similarities than differences, since all wounding is dominated by the secondary injury process of inflammation. As the animal study was formulated, Drs. Gottlieb, Van Meter, and I launched the Perfusion/Metabolism Encephalopathies Study. In this study we would evaluate patients with any chronic cerebral diagnosis, characterize the injury with high resolution SPECT brain blood flow imaging, cognitive testing, pre/post treatment video exams, and symptom questionnaires, and treat them in blocks of 40 Treatments. The basis of the study was to see if the sequence of SPECT brain blood flow scan, single HBOT at 1.5 ATA, and repeat SPECT scan could predict who had injured brain tissue that could respond to repetitive HBOT. In addition, the study would see if clinical improvements could be captured on repeat SPECT scans after blocks of 40 treatments. This “scan, dive, scan” sequence was the provocative test published by Dr. Neubauer in the Lancet in 1990 in a chronic stroke patient, herein characterized as “The Neubauer SPECT Sequence.” His Letter to the Editor was dubbed “The Idling Neuron Letter” because it suggested that injured brain tissue, like other injured tissue in the body, could exist in a low metabolic state for years. The idea was kin to the stunned myocardium concept.
Over the course of the next five years we investigated a large number of patients spanning nearly forty different neurological diagnoses and testing the “Neubauer SPECT Sequence”. The major findings of this experience were that: 1) The Neubauer SPECT Sequence, when impeccably performed, could indeed predict with alarming accuracy who would improve with repetitive blocks of 40 treatments, 2) The clinical, cognitive, and imaging improvements could be documented after 40 treatments, but were generally more significant after 80 treatments, 3) Forty treatments were necessary to achieve durability of the improvements, 4) Chronic TBI was among the most responsive of all diagnoses to this therapy, 5) There was a time-dose dependent limit to the number of blocks and number of HBOT’s that patients could tolerate without serious side effects, and 6) This limit varied with the patient, the pathology, and other factors. Essentially, we had replicated what Neubauer had posited, quantified and refined his approach, and made advances with the application to a variety of other diagnoses including CP, autism, genetic disorders, toxic brain injury, chronic carbon monoxide poisoning, neonatal ischemic/hypoxic brain injury, and thirty-five or so other diagnoses.
Government Access and a Wider Audience
By 2001, we had amassed hundreds of cases and had the good fortune of meeting William A. Duncan, Ph.D., through George Howard, Ph.D., the statistician on our acute stroke/ HBOT project. After successful treatment of one of Dr. Duncan’s family members who was medically disabled from the military due to the persistent post-concussion syndrome from five concussions, the potential of HBOT 1.5 ATA began to reach a larger audience. Dr. Duncan, a congressional legislative staffer in charge of health affairs, secured an invitation to present the science of HBOT in chronic brain injury to a select audience of researchers from the neurological divisions of the NIH. In February, 2001, I presented the scientific argument for HBOT in chronic brain injury and asked for a critique. Shockingly, from the best and brightest there was no critique, no fatal flaw. Armed with this lack of condemnation from arguably the pinnacle of neurological expertise, Dr. Duncan and I proceeded to the FDA, CMS, multiple divisions of the NIH, and a panoply of government agencies and institutions that included physicians from Walter Reed and Bethesda Naval Hospital. Simultaneously, we founded the International Hyperbaric Medical Association and Foundation with Ken Locklear to advance hyperbaric medicine beyond the self-imposed confines of the U.S. hyperbaric community.
Application of HBOT 1.5 to Veterans with TBI and PTSD
By 2004, I had treated over 60 chronic TBI cases of all severities and prepared an NIH grant application for a randomized controlled trial of HBOT 1.5 ATA. While the application was rejected, Dr. Duncan and I traveled to Walter Reed Hospital to introduce HBOT 1.5 ATA to military brain injury casualties. My offer to treat a group of brain-injured Veterans at my expense with Walter Reed testing pre and post HBOT was rebuffed. Subsequent attempts over the ensuing four years were similarly rejected at many levels by Military Medicine as Dr. Duncan, Steve Reimers, and I made multiple proposals and offers to treat Veterans and prove the effectiveness of HBOT 1.5. In the Spring of 2007, we peripatetically sought a congressional appropriation to do a national trial of HBOT 1.5 in the rising Veteran population with TBI and PTSD. In the midst of our efforts the Walter Reed scandal broke and prompted President Bush’s appropriation of $300 million for Veteran TBI and PTSD research. Congressional reaction to our request for an appropriation was sympathetic, but we were redirected to seek the Bush money before any earmark could be justified. I quickly submitted an application to this Congressionally Directed Medical Research Program (CDMRP), and it was unceremoniously rejected.
Stymied and stifled by Military Medicine’s resistance to HBOT 1.5, it became apparent that government funding for an investigation of HBOT 1.5 by me in military Veterans would be impossible. Progress would only be achieved with prima facie evidence at our personal expense. In late 2007, I issued an open offer to treat brain injured Veterans for free to demonstrate to the military that we had a solution for the vexing problem of blast-induced TBI. (Simultaneously, the first blast-induced post-concussion patient, a reserve Army Brigadier General and Florida judge, Patt Maney, was receiving the 80 HBOT 1.5 protocol, now known as the Harch Protocol, in Washington, D.C., courtesy of the efforts of a hyperbaric colleague in Florida who was a family friend of the general, Dr. Eddie Zant). My open offer was transmitted by Dr. Duncan to USA Today where a Boston magistrate answered on behalf of his brain injured son. Within a few months through the personal donations of my partners Drs. Paul Staab and Dr. Keith Van Meter, and myself, we began treating this 25-year-old Marine machine gunner. This Marine was debilitated with the post-concussion syndrome (PCS) and post-traumatic stress disorder (PTSD) from seven brain-rattling improvised explosive device (lED) explosions.
After forty HBOT 1.5 ATA treatments, his headaches were eliminated, his cognitive deficits improved, and to our surprise, his PTSD was gone. The case was reported in BioMed Central’s Cases Journal: www.hyperbaricmedicalassociation.org/406/text/610/files/Ins3_HBOT1_5_Harch_Cases_Journal_20090609_Compressed.pdf. Four additional cases followed in rapid succession with similar results. The experience with chronic non-blast TBI of the past 18 years was now replicated in blast induced TBI.
With the assistance of Dr. Duncan and the Honorable Martin Hoffmann, ex-Secretary of the Army under Gerald Ford and close personal friend of the restored general and judge, Patt Maney, awareness of the potential of HBOT 1.5 was raised to the level of common knowledge in Washington, D.C., by 200 visits to House and Senate offices in the Spring and Summer of 2008. This advocacy was formalized in a congressional earmark submitted by Louisiana Congressmen Alexander and Melancon and Senators Vitter and Landrieu to fund a national multi-center study of HBOT 1.5 in military Veterans with blast-induced PCS and PTSD. The earmark and study were sponsored by the International Hyperbaric Medical Foundation and were to be administered by LSU School of Medicine, New Orleans. Known as the National Brain Injury Rescue and Rehabilitation Project (N-BIRR), the appropriation was approved in the summer of 2008, and was awarded on September 29, 2010.
This advocacy also had the unintended consequence of congressional pressure on Military Medicine to address the potential for HBOT 1.5 in brain injured Veterans. The Navy Surgeon General, Admiral Robinson, responded with a request for me to present the science of HBOT and my experience treating chronic TBI/PCS. On August 14, 2008, I made a presentation to Admiral Robinson, the Assistant Commandant of the Marine Corps (now the Commandant), advocates of HBOT 1.5 such as the wife of the Chairman of the Joint Chiefs of Staff, the wife of the Commandant of the Marine Corps, representatives of three congressional offices, neurologists, neuropsychologists and brain injury specialists from the Navy SG’s office, Dr. Duncan, a variety of other military brass and medical experts including a military hyperbaric physician expert, and three of the five brain-injured Veterans I had treated. I made a plea for funding the pilot trial of HBOT in PCS and PTSD that was under review by the LSU School of Medicine’s Institutional Review Board. I was assured by the Navy SG that “funding is the least of your problems, Dr. Harch.” He announced that they had $900 million to fund research and that the $600,000 I was seeking was a pittance. Not a dime was forthcoming, however. Instead, I was asked to work with his group to plan “the best way forward.”
In the ensuing sixteen weeks, I worked with his staff, but was excluded from the planning of the summit Department of Defense Consensus Conference on HBOT in TBI that occurred on December 5-6, 2008, in Arlington, Virginia. Unbeknownst to me and any of our team, the president of the UHMS had sent a private letter to the Navy Surgeon General (SG) and other military officials one week before my presentation to the Navy SG claiming that the UHMS Hyperbaric Oxygen Therapy Committee Report was the “Gold Standard” in diving and hyperbaric medicine. The letter proposed that ” … the DoD support the UHMS in convening an ad hoc expert panel to review the available literature investigating HB02 as a therapeutic option in TBI and other combat injuries.” Eight weeks later this letter was announced. Interestingly, the two most authoritative and experienced clinicians in the field of HBOT in acute and chronic TBI were not on this expert panel.
On December 5, 2008, I presented the science of HBOT 1.5 in chronic brain injury and the results of now the first five subjects I had treated in the pilot trial, including high-resolution functional brain imaging. The imaging was independently validated by the conference’s chosen imaging expert, professor and ex-chairman of radiology, Dr. William Orrison. I also announced the congressional earmark that had been awarded at a lower amount than requested and my need for funding for both the pilot trial and N-BIRR. These requests were ignored. At the conclusion of the meeting, General Loree Sutton, the director of the DoD Centers of Excellence for Psychological Health and Traumatic Brain Injury, gathered the N-BIRR team to inform us that the Consensus Conference’s conclusion of a proposed randomized trial over the next 3-5 years was unacceptable. She wanted testing of HBOT 1.5 and the Harch Protocol now. These brain injured service members could not wait, in her opinion. She invited us to share our plans for the national multi-center study.
Formally excluded from the DoD process and without funding, the N-BIRR team initiated a fundraising campaign that over the subsequent sixteen months raised the $593,000 necessary to complete the LSU pilot trial. By the Fall of 2009, we had treated and collected data on 15 subjects and presented the results at the 8th World Congress on Brain Injury in Washington, D.C. The abstract can be viewed at: https://ibia.conference-services.net/reports/template/onetextabstract.xml?xsl=template/onetextabstract.xsl&conferencelD=1677&abstractID=359999. The statistical analysis of the data is significant for nearly every measured outcome parameter. Veterans achieved symptomatic, physical exam, cognitive, quality of life, and functional imaging improvements in one month of HBOT 1.5, the first half of the Harch Protocol. Full scale I.Q. improved by 15 points, the difference between a laborer and an engineer, working memory by 25 percentile points, attention/concentration by a similar amount, while post-concussion symptoms decreased by 40%, PTSD symptoms by 30%, and depression by 51%. The patient’s quality of life scores increased by 40% and their self-reported cognitive, physical, and emotional well-being improved by 33-90%. Despite the absence of a control group, the magnitude of these improvements has never been demonstrated with placebo effects.
Further evidence against a placebo explanation of this data was the functional brain imaging which showed significant improvements after the first hyperbaric treatment for every gray and white matter site measured in the brain. This imaging data thus validated The Neubauer SPECT WCHM -33 Sequence. In addition, after 40 hyperbaric treatments, significant improvements were seen in 50% of the white matter sites, consistent with direct treatment of the primary injury site in mild-moderate TBI. Lastly, the magnitude of improvement in memory was nearly identical to the magnitude of improvement in the Morris Water Task of the rat TBI experiments published in Brain Research. Essentially, HBOT 1.5 was duplicating in U.S. Veterans with blast-induced PCS similar effects that it had generated in other causes of chronic PCS and the animal model. In addition, it was showing benefits in functional imaging and in reduction of PTSD just as it had in the Boston Marine machine gunner two years before.
Independent Clinical Confirmation of HBOT 1.5 in Veterans with TBI/PCS
Since the pilot trial began in September, 2008, Dr. Eddie Zant, of Ft. Walton Beach, Florida, has used the Harch Protocol in a dozen subacute brain injured U.S. Veteran airmen from the Iraq and Afghanistan Wars. The results are the same as those we have achieved in the pilot trial, with the added benefit that most of the airmen have been able to return to active duty. This benefit is due to a shorter delay to treatment, namely, months, instead of the average 2.7 years in our study. Dr. Zant’s experience also replicates our original findings with brain decompression illness patients. Specifically, treatment of the subacute and chronic brain DC\ patients was dose dependent, protracted, and less successful than the published results of the world’s navies where first recompression cured over 90% of patients treated within the first hour of injury. This confirmation of effect by an independent physician strengthened the validity of the data in the pilot trial. Two of Dr. Zant’s cases were published last year with referring hyperbaric physician and retired Air Force Colonel Jim Wright: Wright JK, Zant E, et. al., “Case Report: Treatment of mild traumatic brain injury with hyperbaric oxygen.” UHM, 2009; Vol. 36(6):391-9.
Purpose and Implications of the Above Chronology
The purpose of reciting the details of the above chronology is to underscore the importance of the solution that I propose for proofing HBOT 1.5 in blast-induced PCS/TBI and prepare readers for the possible negative consequences of the planned studies of the Department of Defense on this subject.
For the past 40 years, there has been a concentrated effort by a small number of individuals to advance the science of HBOT in chronic brain injury. The protocol for treatment of chronic TBI has been refined during these decades and a substantial portion of this information was shared in a goodwill effort to obtain funding for a definitive study on HBOT. Unfortunately, that information has been used by the DoD to formulate a series of studies performed by a group of individuals who have little or no experience with HBOT in chronic brain injury, especially blast-induced chronic brain injury. The DoD’s proposed protocol for definitive proofing will use a hyperbaric air treatment in the control group that has never been tested in adults with chronic TBI and that is similar to a protocol that has been shown to be effective in children with cerebral . The pressurized air has an increased amount of oxygen and pressure that effectively constitutes an alternate dose of hyperbaric oxygen. Whether this is a deliberate design flaw or indicative of the absence of experience/knowledge of the investigators, should the two groups have equal treatment effects as they did in the 2001 Collet Lancet CP/HBOT study, it will effectively negate the possibility of institutional application of HBOT for PCS to any Veteran.
Should the study have positive results for the HBOT 1.5 group, based on the behavior and statements of military officials in our struggle to advance HBOT 1.5 for chronic TBI in the past nine years, it is possible, and in my opinion likely, that the true results will never be published. My candor and conviction in this matter stems from the multiple attempts by Military Medicine to inhibit, obstruct, condemn, and discredit the LSU Pilot Trial, our exclusion from DoD funding, and the most recent example of suppression of scientific evidence in the Cognitive Stability Index (CSI) study. As recounted in Government Executive (www.govexec.com/story_page.cfm?filepath=/dailyfed/0510/052410kp1.htm&oref=search), a study performed in Iraq in 2006-2007 by Air Force physicians that proved the superiority of a commercially available acute TBI screening tool (CSI) to the military’s ANAM has still not been published. No one knows what has happened to the data, but one of the investigators, Dr. Gerald Grant, Associate Professor of Pediatric Neurosurgery at Duke University says that the final manuscript has to be approved by the Air Force and Army, and he doesn’t believe that they will approve it. It is easy to understand, given the history of the military’s hesitant acknowledgement of the TBI epidemic in active duty service members, that a more sensitive tool to detect acute TBI would increase the already huge numbers of TBI-affected Veterans. That would not be well received.
The other reason that proof of effectiveness of HBOT 1.5 will likely not be published or possibly be corrupted is the feared price tag of treating hundreds of thousands of brain injured service members with a treatment that is billed at $2,000/hour in private sector hospitals. That fear was just openly expressed by retired Army Colonel Frederick Flynn, head of the TBI program at Madigan Army Medical Center in Washington state, in Navy Times (Marine Corps’ Edition) September 13, 2010, edition, “It is very, very expensive therapy and once you jump on the bandwagon that [hyperbaric oxygen therapy] unequivocally treats and cures the symptoms associated with mild TBI, it is going to cost the American taxpayer an awful lot of money. So, we need to be right before we take that big step.” The reality is that HBOT costs about $200/treatment at freestanding facilities and far less in the military.
A Solution
The LSU Pilot Trial finished in late September. Data should be analyzed and available in a few months. Meanwhile, the template of the pilot trial has become the foundation of the protocol for N-BIRR, the multi-center national project where both Veterans and civilians with chronic TBI will be able to obtain the Harch Protocol. N-BIRR has a number of critically important features: 1) It will be administered by the independent International Hyperbaric Medical Foundation and our team; 2) It is fully approved by Western IRB; 3) The data will be electronically logged by each center to a contracted web-based service licensed to the IHMF; 4) All subjects will receive HBOT 1.5; there will be no placebo control group; and 5) The study will incorporate the modern Bayesian Statistical Method that uses accruing results to calculate statistical proof of efficacy.
Approximately 15 sites are now approved for N-BIRR, and a number of these sites are actively treating patients. The exciting facet of N-BIRR is that with funding and adequate recruitment, this study can be completed in one year or less. Meanwhile, the limited congressional appropriation for LSU will fund a randomized trial of half of the Harch Protocol at LSU School of Medicine, New Orleans. It is anticipated that these studies will be able to offer a new indication for HBOT and hope for the hundreds of thousands of brain injured U.S. Veterans.
Patient Consent Disclaimer: Patient consent was obtained for all patients named in this article.