Multiple Sclerosis – A 1994 Case Study
October 19, 2021Near-drowning victim experiences “miraculous” recovery
November 15, 2021Case study: Delayed treatment of traumatic brain injury and PTSD. Rusty is a 45 year old man who had been in the military and was back in civilian life, a family man, serving as a law enforcement officer, and running a small business in the Midwest when 9/11 occurred. Outraged by the 911 attacks he reenlisted and found himself in Iraq, escorting translators around the Green Zone. In a barrage of more than 300 rounds of enemy mortar he was knocked unconscious.
In the aftermath he suffered from debilitating headaches, vertigo, short-term memory loss, and constant fatigue, was medically boarded out of the military, and erroneously diagnosed with a psychiatric disorder. One year later, a military caseworker happened to note his symptoms and called Dr. Harch. Dr. Harch screened him over the phone and took a detailed history. It was determined that Rusty had persistent postconcussion syndrome and met inclusion criteria for entry into Dr. Harch’s LSU veterans’ TBI study.
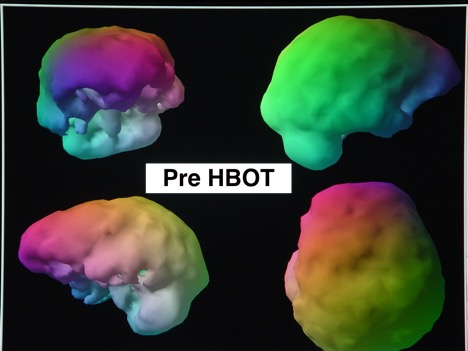
One test in the study involved SPECT brain blood flow imaging and the resulting images were dramatic, in fact, the most exceptional of any of the 30 participants in the study. The entire left side of his brain showed a reduction in brain-blood flow (the side on which the mortar blast had occurred). He also complained about intense itching and periodic blistering on his left arm. Dr. Harch suspected shrapnel and X-rayed his arm, discovering 16 pieces of embedded metal. Here was the evidence that he had experienced a concussive blast injury. Over the course of treatment, his symptoms and imaging improved. He was eventually awarded a Purple Heart and now serves as liaison to the North Dakota State Legislature on matters related to veterans.
SPECT brain blood flow scan before HBOT:
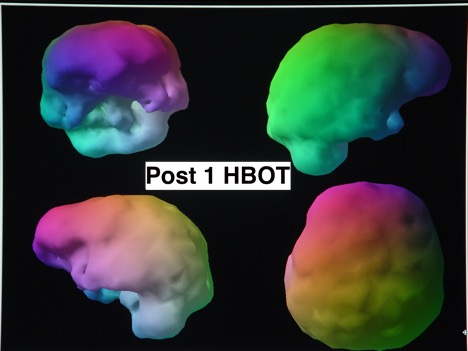
SPECT scan after the first HBOT:
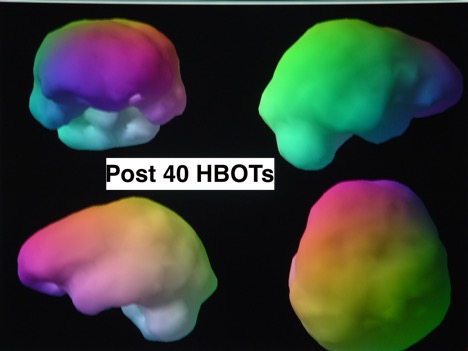
SPECT after 40 HBOTs: